Each year, more than 33,000 Europeans die from infections caused by bacteria that have become resistant to antibiotics. This impact on population health is already similar to the increased impact of three major infectious diseases: influenza, AIDS and tuberculosis. This is one of the main findings of an extensive survey conducted by the European Center for Disease Prevention and Control (ECDC).
The study, the agency’s largest to date, highlighted that in 39 percent of cases, the bacteria involved were already immune to so-called “last-line” antibiotics such as mucin and carbapenems. According to the ECDC, this situation is “very worrying because these antibiotics are the last available treatment”. “When [these drugs] are no longer effective, treating these infections is very difficult and in many cases impossible,” the agency said. The study insists that the cause of these drug resistance is misuse of antibiotics and inadequate measures to control and prevent infections.
The study was based on data collected throughout 2015 from the European Union and a large network of hospitals in Norway and Iceland. Based on this information, the authors used mathematical estimates to calculate that there were 670,000 infections caused by multi-drug resistant bacteria in that year, and that “as a result” 33,110 patients died. These estimates take into account projections for the total population of the countries studied and the mortality rates attributable to each bacterium, as well as many other variables.
The most striking novelty of this work is that it is the first study of its kind to count the number of years lost to disease, disability, or premature death (DALYs). This measure reveals large differences between the countries surveyed. If Europe has an average of 170 years per 100,000 inhabitants, Italy and Greece easily exceed the 400 years lost, while Norway, the Netherlands, Estonia and Iceland are below 40 years.
“The finding of 170 DALYs per 100,000 inhabitants is similar to the sum of the population impact of three major infectious diseases such as influenza, tuberculosis and AIDS,” the study notes.
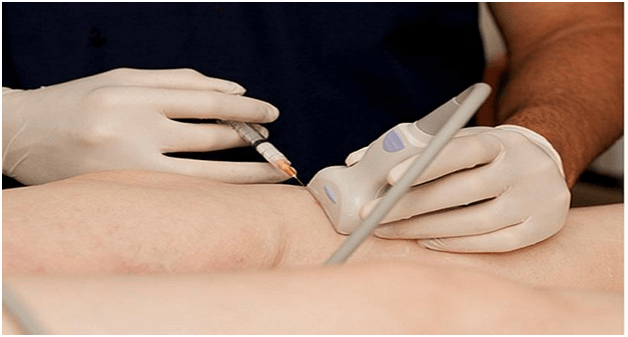
The authors of the study stressed that almost two thirds of the infections, 63.5% of the total, were “acquired in the health system”, mainly in hospitals, through the application of prevention and control in the health sector, which offers “much room for improvement” centers. “.
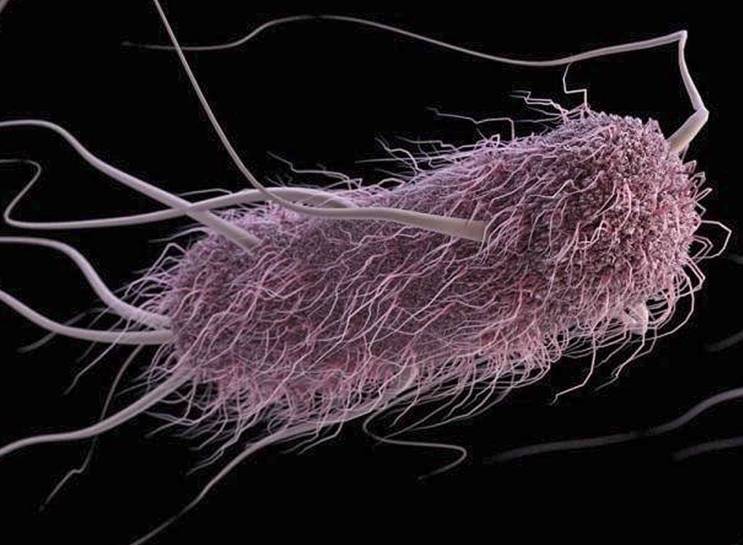
The main bacteria involved are known to health professionals, such as Enterococcus faecalis and Enterococcus faecalis, Klebsiella pneumoniae, Staphylococcus aureus (MRSA) and Streptococcus pneumoniae. These are very common pathogens that were initially sensitive to all antibiotics, but have developed immunity to several in recent decades.
The work was done by ECDC experts in collaboration with dozens of European experts and has been published in the reference journal The Lancet Infectious Diseases. The authors acknowledge the limitations of their work due to the complexity of the mathematical estimates made, but refer to the European Antimicrobial Resistance Surveillance Network (EARS-Net). The experts also defend “the systematic evaluation of the most recently published studies to obtain the best estimates of mortality from multi-drug resistant bacteria and their complications”.
According to the ECDC, the goal of this work is to provide the European authorities with up-to-date information to address the “need for close coordination among all the countries studied, as well as on a global scale. However, given the significant differences observed between countries, the ECDC urged “reduction of disparities through appropriate prevention and control measures” as well as “precise management of antibiotics. “All of this,” he concluded, “must be a priority goal for all countries.